Oncology
What if you could orchestrate clear care pathways for every patient?
What if you could bring the right people together with the right information at the right moments in time, orchestrating clear care pathways for each stage of the patient journey? This could benefit not only the part of the oncology patient journey that involves diagnosis and therapy, but it could help in using diagnostic data to select the optimal treatment or plan, preparing the treatment plan (surgery, focal therapy, radiation oncology) and in ongoing assessment and follow-up care.
What would it look like if we could make patient care pathways clearer, and in doing so, shorten the time to diagnosis and treatment, improve the patient and staff experience and, ultimately, aid patient outcomes? This article looks at integrating multidisciplinary efforts along the patient journey.

At a glance
Challenge Cancer care is increasingly complex, with novel diagnostics, new treatment options and a multidisciplinary approach to oncology care organization.
Solution Orchestrate decision-making at every pivotal moment of the patient’s oncology care pathway.
Results Providing clear pathways in order to treat cancer as early as possible and in a coordinated way has positive effects on outcomes and costs.
Share this article
Oncology treatments are evolving faster than clinical teams can adapt
Cancer care is becoming more complex by the day, with ever-more refinement in tumor characterization, more therapy options, and an increasing number of multidisciplinary specialists engaged in patient care. Patient complexity is also increasing, and clinicians are challenged to coordinate across specialties, identify all appropriate treatment options and select the right care pathway for each patient.
40%
of patient treatment plans changed after a multidisciplinary tumor board review1
60%
of patient staging and assessment recommendations changed after a multidisciplinary tumor board review1
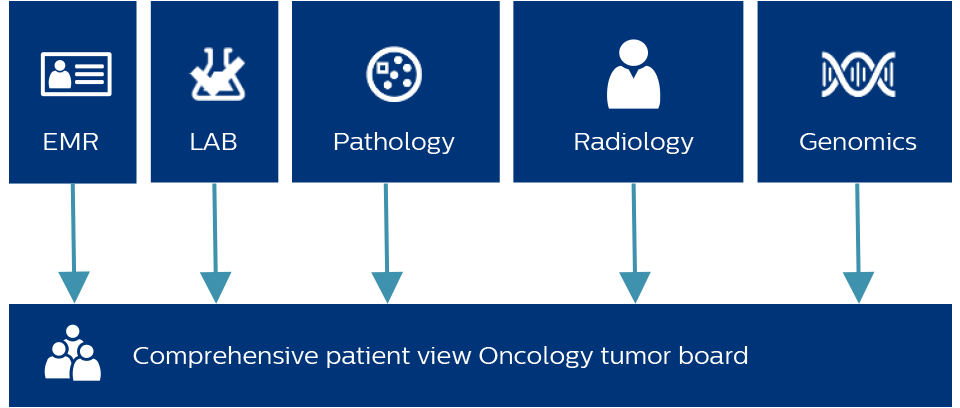
What does it mean to integrate data across specialties?
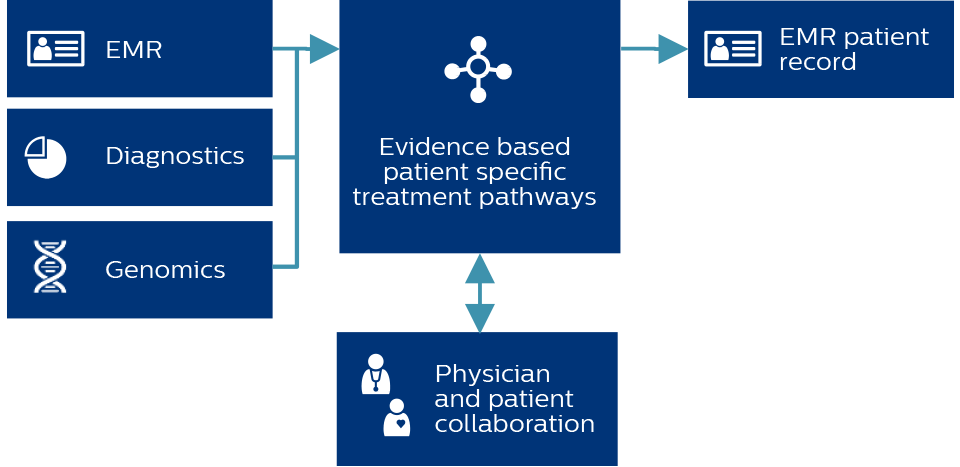
By integrating data across specialties and delivering insights directly to clinical teams, care pathways are streamlined and patient care can be orchestrated with the speed, efficiency and patient-centered approach that cancer care demands. We must provide timely access to relevant information to the multidisciplinary team.
More specialties are involved in the care of a cancer patient than ever before. Multiple patient handoffs, inefficient workflows across specialties and incomplete patient data can result in missed or imprecise diagnosis. These challenges can also delay the start of treatment, and cause missed opportunities for early intervention and adjustment of treatment plans. All of this impacts patient and staff satisfaction, and potentially quality and outcomes.
Dr. Pieter Postmus talks about the need for near-instant access to information
I need to have all the information that is available within, let’s say, a few seconds on my screen, preferably a double screen just to compare things while not having to switch from one document to another one…the plan includes quite often that we need to discuss it in a multidisciplinary setting as well, so is everything available to those who are participating?"
Professor Pieter Postmus, MD, PhD
Head of Department and Professor of Pulmonology, Leiden University Medical Centre
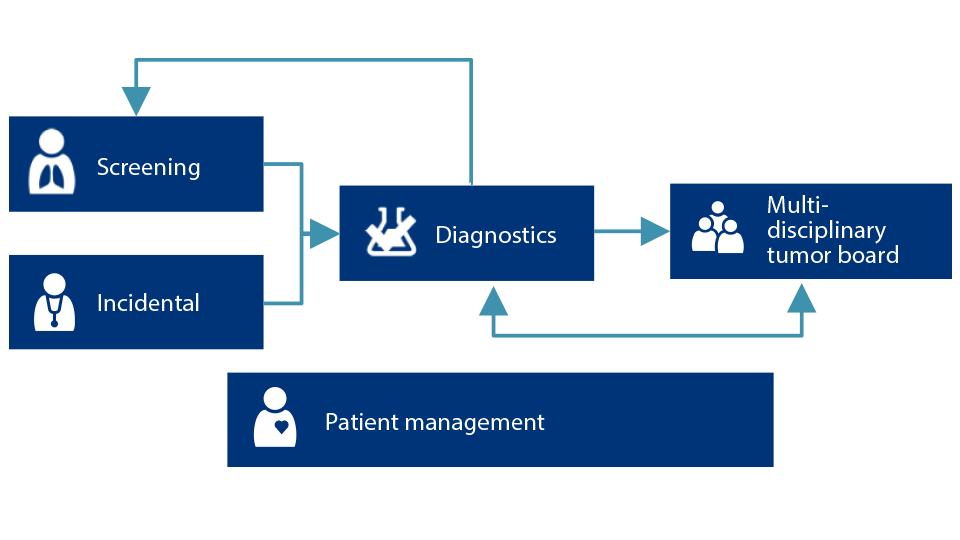
You’ve screened for lung cancer…now what?
To coordinate and manage an effective lung cancer screening program requires simultaneously handling a wide variety of tasks on a daily basis. Determining who is eligible, notifying and scheduling follow-ups, and reporting program status can be labor-intensive – and potentially risky if details are overlooked. Further complicating the situation? Many lung cancer screening workflows only screen and treat patients with explicit symptoms of cancer, but that misses patients with incidental nodules identified outside of the screening program imaging.
Screening for lung cancer and orchestration of follow-up on incidental findings provides excellent examples of the need for coordination. When lung nodules are found, the lack of infrastructure, coordination and capacity to manage patients in a timely manner can lead to delays in diagnosis and treatment.2
Lung cancer is the leading cause of cancer-related deaths3
70%
Of all incidental lung nodules are not followed and managed appropriately2
25%
Incidental nodules have an approximate 25% malignancy rate, risk stratified, compared to approximately just two percent within the typical screening population.4,5
30%
Of those incidental nodules, only approximately 30% are followed and properly managed.2
92%
Early diagnosis and immediate resection leads to 92% survival at 10 years6
Now you can simply track patients through their journey
Philips Incidental Nodule Manager helps identify suspicious pulmonary findings in patients who might otherwise be overlooked. It uses Natural Language Processing to mine radiology reports for the relevant keywords to trigger referral for follow up, management and treatment. With multiple checks and balances in place, Philips aims to help ensure patients are not lost to follow-up. Let’s look at how having the right information at the right time supports treatment selection and the power of patient reported outcomes connecting the doctor and patient during treatment and assessment.
The need is clear for a simplified, automatic tool to track patients through their oncology journey. Philips Lung Cancer Orchestrator helps you identify and provide follow-up for more patients, streamline workflows, and makes management of lung cancer screening programs easier – providing the right information when you need it.
A clear pathway starts with the right information
Philips Oncology Pathways powered by Dana-Farber Cancer Institute delivers high-quality, detailed, evidence-based treatment protocols and can serve as an important tool in improving care quality and reducing costs. Based on the captured patient information, the clinical user is able to navigate through the branches of the pathways to make clinical decisions and provide a treatment plan recommendation including clinical trials.
“The need for oncology pathways rings true for me every day,” Dr. Jackman says. “We wanted to address the complexity, cost and coordination of cancer care as we tried to spread care over a larger network. We were looking for a solution that would codify best practices, support decision-making in real time to reduce unwanted variation, emphasize accrual for clinical trials, and oversee care as well as capture data from across our network.” - Dr. David Jackman
Dr. David Jackman on bringing greater efficiency to cancer care
When we think about the future of healthcare, and how we make all of this more efficient, how do we improve collaboration and communication? How do we bring the right people together with the right information? And how do we do this all in as seamless a way as possible?"
David Jackman, MD
Medical Director of Clinical Pathways, Dana-Farber Cancer Institute
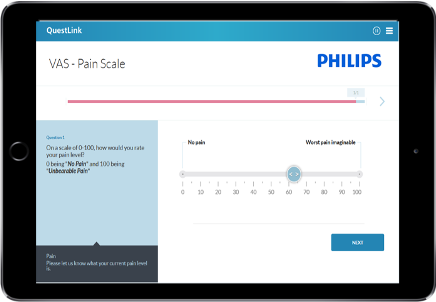
Connecting clinicians and patients with actionable data
Some institutions are turning to digital solutions such as Philips QuestLink to collect, process and analyze outcome data such as patient reported outcomes (PROs). Capturing and reporting this data across entire care pathways through automated online patient survey instruments supports the evaluation of care effectiveness, more personalized treatment, and it helps provide actionable health data before, during and after treatment.
Start as soon as possible and find what matters to your patient, because those are the most important outcomes."
Dr. Detlef Loppow
Managing Director of the Martini-Klinik
Bringing the right people together with the right information
It is possible to improve collaboration across specialties and with patients to bring the right people together with the right information to orchestrate clear care pathways. Philips works with you to understand your specific requirements and tailors planning, implementation and training to assure staff proficiency.
How Philips can support you
Philips Lung Cancer Orchestrator
Integrated lung cancer patient management system
Philips Oncology Tumor Board
Integrated diagnostics for a comprehensive patient view
Go deeper
Are you interested in learning more about how these solutions can help you address your challenges?
Video
Philips Lung Cancer Orchestrator
Philips Oncology Pathways Guide powered by Dana Farber Cancer Institute
Empowering oncologists in their treatment decision journeys
Go deeper
Are you interested in learning more about how these solutions can help you address your challenges?
Article
Read the Expert Perspectives article on “Philips Pathways Navigator powered by Dana-Farber Cancer Institute”
Video
Watch Dr. David Jackman on disrupting healthcare to provide access to best practices in cancer care.

Get in contact with our Oncology specialists
Share this article
At a glance
Challenge Cancer care is increasingly complex, with novel diagnostics, new treatment options and a multidisciplinary approach to oncology care organization.
Solution
Orchestrate decision-making at every pivotal moment of the patient’s oncology care pathway.
Results Providing clear pathways in order to treat cancer as early as possible and in a coordinated way has positive effects on outcomes and costs.
Share this article
Other challenges you might be facing
See what other thought leaders have to say

More information about Oncology Solutions
Find out how Philips can help you enable a clear care pathway with predictable outcomes for every patient.
1. Schmidt HM, Roberts JM, Bodnar AM, et al. Thoracic multidisciplinary tumor board routinely impacts therapeutic plans in patients with lung and esophageal cancer: a prospective cohort study. Ann Thorac Surg. 2015;99(5):1719-1724. doi:10.1016/j.athoracsur.2014.11.019 2. Blagev DP, Lloyd JF, Conner K, et al. Follow-up of Incidental Pulmonary Nodules and the Radiology Report; J Am Coll Radiol 2014;11:378-383. 3. International Agency for Research on Cancer, World Health Organization. Press Release N° 263. Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018. 12 September 2018. 4. Gildea TR, DaCosta Byfield S, Hogarth DK, Wilson DS, Quinn CC. A retrospective analysis of delays in the diagnosis of lung cancer and associated costs. Clinicoecon Outcomes Res. 2017;9:261-269. 5. Estimated for illustrative purposes based on various assumptions and expectations using: Advisory Board. Lung Cancer Screening Volume and Revenue Calculator. November 18, 2014. Updated April 12, 2016. Available at www.advisory.com/research/imagingperformance-partnership/resources/2014/lung-screeningtoolkit/lung-cancer-screening-calculator. Last accessed August 3, 2020. 6. International Early Lung Cancer Action Program Investigators. Survival of patients with stage 1 lung cancer detected on CT screening. N Engl J Med. 2006;355:1763- 1771 DOI: 10.1056/NEJMoa060476